As Community Health Centers (CHCs) mark 60 years of service, it’s time to reflect not on just their legacy, but their future.
These frontline institutions have become lifelines for 1 in 10 nationwide. Nearly 1,500 CHCs operate in over 16,000 urban and rural communities, serving 32.5 million people, including Medicaid beneficiaries, veterans, older adults, and low-income families. They offer integrated medical, dental, behavioral health, pharmacy, and enabling services, and they generate billions in cost savings every year by keeping people healthier and out of the emergency room and hospitals.
But the road ahead is uncertain.
CHCs are confronting intensifying financial and operational pressures as demand for their services rises. The gap between mission and resources is widening. If CHCs are to thrive, philanthropy must step forward with greater intention, scale, and staying power to help shape the future of community health.
CHCs are not just healthcare providers. They are rooted in the neighborhoods they serve. They address health by identifying and responding to real-world challenges that patient face. They screen for food insecurity, housing instability, transportation barriers, interpersonal violence, and other underlying issues. They then act on those findings, connecting patients with local resources and partners. This whole whole-person care model that is provided under one roof is especially valuable for individuals with complex health, behavioral, and non-medical needs.
But that work is under threat. Workforce shortages, rising operating costs, and aging infrastructure are to maintain access and quality. We cannot afford to lose the ground CHCs have gained, especially as CHCs build, test, and expand innovative care delivery models.
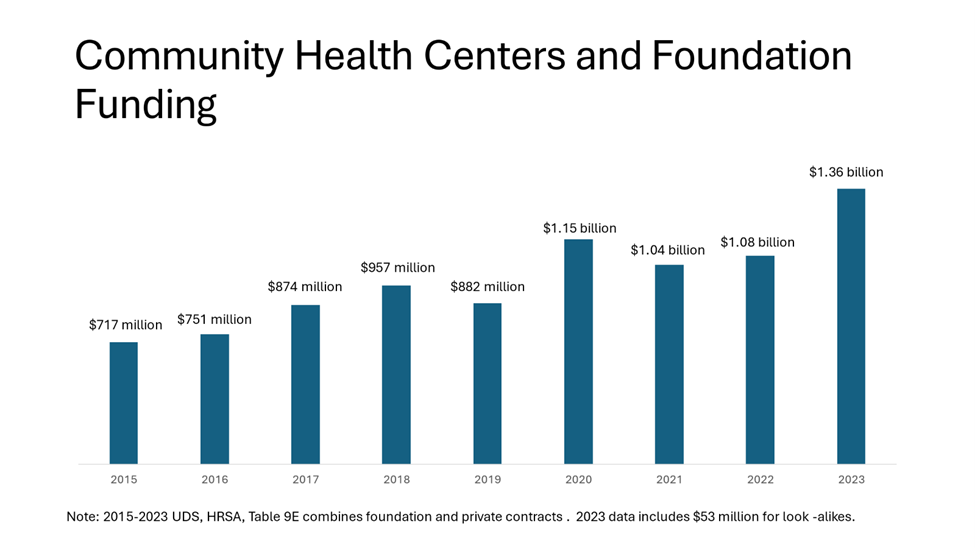
Fortunately, we’ve seen what’s possible when philanthropy steps in. In 2023, CHCs received $1.4 billion in private contributions – nearly double the amount awarded a decade ago. (Figure 1) While this contribution represents just 3% of total revenue, it has had a profound impact. Philanthropic support enables CHCs to test and scale innovations, launch new services, and meet urgent and emerging community needs that the federal and state funds cannot cover. Philanthropic grants also support data and technology upgrades, workforce pipeline and retention strategies, mobile health expansion, chronic disease management, enabling services, and disaster preparedness.
Several notable partnerships have helped drive such innovation. The Robert Wood Johnson Foundation invested over $5 million to help CHCs integrate social needs into patient care – an effort reflected in the fact that nearly 70% of CHCs now screen for food, housing, transportation, and other risk factors. The Lowenstein Foundation provided over a million dollars to advance mobile health growth and development, contributing to the growth of more than one thousand CHC mobile sites nationwide. The Centene Foundation recently committed to the three million dollars to support CHCs transitioning to value-based care and to improve maternal health care. Direct Relief awarded one million dollars to the National Association of Community Health Centers (NACHC) to support CHC access, adding to over one billion dollars in medicine, supplies, and donations it has already provided to CHCs for disaster preparedness, chronic disease management, and preventative care. Corporate partner Abbott is partnering with NACHC to expand CHC digital innovation and nutrition initiatives.
Despite such impactful partnerships, they must become the norm. While CHCs are proven change agents, they cannot continue to do more with less. Strategic investment is needed now more than ever.
So where can philanthropy make the greatest impact?
- Data infrastructure and analytics: CHCs urgently need investments in the tools, systems, and staff to better measure health outcomes, cost avoidance, population needs, and program effectiveness. Funders can support data modernization, – from data migration and integration to data cleaning and warehousing – analytic training, and artificial intelligence integration, enabling CHCs to lead in value-based care and quality reporting.
- Workforce and leadership development: CHCs face severe workforce shortages, especially in rural areas and behavioral health. Philanthropy can help strengthen recruitment, loan repayment, and pipeline programs. But sustaining the CHC mission also depends on cultivating internal leadership and from historically underrepresented communities. Supporting management training, fellowships, and mentorship programs will create a diverse, skilled, and future-ready workforce that can lead CHCs through change.
- Innovation in care delivery: CHCs are natural incubators of innovation, but limited margins restrict their ability to experiment or evaluate new approaches. Funders can support the design and spread of integrated models that combine behavioral health, substance abuse treatment, and chronic care. Support for digital tools, ambient listening, remote monitoring, synchronous care, and virtual group visits will enhance coordination, engagement, and efficiency.
- Research and clinical trials: Critically, CHCs also need support to engage providers and patients in clinical research to ensure that historically underserved populations are represented in evidence generation and benefit from emerging treatments. Philanthropic partnerships can help CHCs participate meaningfully in these initiatives and ensure patients have access to advanced treatment options.
- Emergency response and preparedness: CHCs are trusted responders during disasters, providing stability, care and access in communities with limited health infrastructure. Yet many lack the resources to prepare for or sustain services during emergencies. CHCs need sustainable systems like solar power and HVAC upgrades that can improve care delivery, reduce environmental risks, and expand access. Investments in supplies, equipment, training, mobile capacity, and facility resilience will enable CHCs to remain operational during crisis (or soon after) and serve as essential community anchors.
CHCs have endured and evolved because they are embedded in and accountable to the communities they serve. Over 50% of CHC patients are covered under Medicaid, 18% are uninsured, and 11 percent are enrolled in Medicare. CHCs stretch every dollar and are governed by a patient majority board that ensures investments are responsive and results driven.
What makes philanthropy so powerful is its ability to bridge the gap between what public funding can support and what communities need most. Such investments can unlock new partnerships, de-risk innovation, and help demonstrate impact in ways that attract broader funding and policy support.
As CHCs commemorate six decades of service and impact, we call on philanthropic organizations, including private foundations, corporate funders, and health-concerned investors, to partner with us in securing the future of community health. Together, we can ensure that CHCs not only survive but thrive to deliver high-quality, comprehensive care to the millions of low-income individuals and families who rely on them. Let us work together to build a healthier and more resilient future.





